Antimicrobial resistance is a growing global health problem recognized as n°1 priority by the WHO. It is estimated that 5-10% of hospital patients in US and Europe develop a hospital-acquired (nosocomial) infection, with > €30 billion additional annual costs to public health and > 100,000 deaths due to drug-resistant bacterial infections. In 2019, 1.3 million people died from drug-resistant infections, and antimicrobial resistance is predicted to kill > 10 million people every year by 2050.
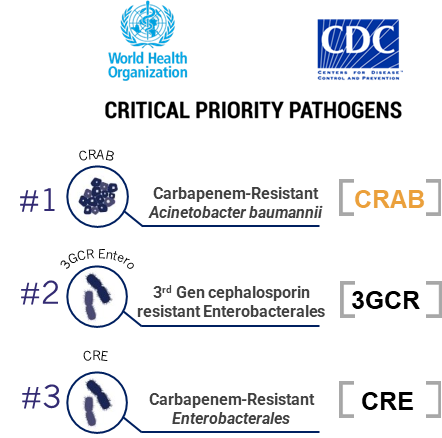
Current antibacterial chemotherapy is increasingly compromised due to the spread and transfer of genes which encode resistance factors. The main resistance mechanism associated with high-level resistance to carbapenems is the production of certain types of β-lactamase enzymes (known as carbapenemases) which are able to destroy them. The most widespread carbapenemases are the KPC and OXA-type serine β-lactamase enzymes.
Many β-lactamase inhibitors have been developed (either marketed or in late-stage development) which inhibit some of these enzymes in certain bacteria but none show clinically relevant coverage against KPC or OXA-producing carbapenem-resistant Enterobacterales (CRE) as well as OXA-producing carbapenem-resistant A. baumannii (CRAB). Better inhibitors are required to restore the effectiveness of carbapenem antibiotics.